Enhancing concussion care in Colombia

BCIRPU Director Dr. Shelina Babul travelled to South America this past Spring to improve concussion care and education in Colombia.
The goal of the trip was to help healthcare professionals understand the latest in evidence-based care for concussion diagnosis and management, and highlight prevention efforts. Dr. Babul spent a week in Medellín with Dr. Mauricio Garcia-Barrera, Professor of Psychology and Associate Dean of Research and Graduate Studies at the University of Victoria. Dr. Garcia-Barrera is a clinical neuropsychologist who leads the CORTEX Lab, which is dedicated to the analysis of human behaviour and executive brain function.
In Colombia, Drs. Babul and Garcia-Barrera delivered a three-hour workshop on concussion followed by an introduction to the Concussion Awareness Training Tool (CATT) e-learning course for Medical Professionals. In attendance were individuals from graduate training programs across several health-related fields and medical schools. They also connected with several researchers and graduate students to discuss research and opportunities for collaboration.

In preparation for this trip, the CATT website and its Medical Professionals course was translated into Spanish. CATT is already available in English and French, and work is ongoing to translate CATT into Arabic.

Medellín, the “City of Eternal Spring,” is the second-largest city in Colombia and Dr. Garcia-Barrera’s hometown.
“In Colombia, concussions are not top of mind for medical professionals,” said Dr. Garcia-Barrera. “We’re hoping to change that. We want to increase awareness and educate healthcare professionals on how to identify, diagnose, and manage concussions in Colombia.”
Universidad CES was the host university in Medellín. Participating organizations included: Universidad de San Buenaventura, Grupo de Neurociencias de Antioquia, and Universidad Pontificia Bolivariana.
This wasn't the first time that CATT has been presented globally. Dr. Babul has delivered CATT workshops to medical professionals in East Africa, South Africa, and Lebanon. In Lebanon, Dr. Babul and BCIRPU Investigator Dr. Ian Pike worked with colleagues to form the ICARE program in 2023, which provides school nurses with the knowledge and protocols needed to respond to concussions in educational settings.

“CATT was built for a global context,” said Dr. Babul. “How we diagnose, treat, and manage concussions should not be different across the globe. I’m excited to introduce health care providers in Colombia to evidence-based standards for tackling the issue of concussions.”
Dr. Babul also took some time to enjoy the food and sights that Colombia has to offer. She travelled within Medellín, going to Bogota and Cartagena, and then went over to Peru for vacation.
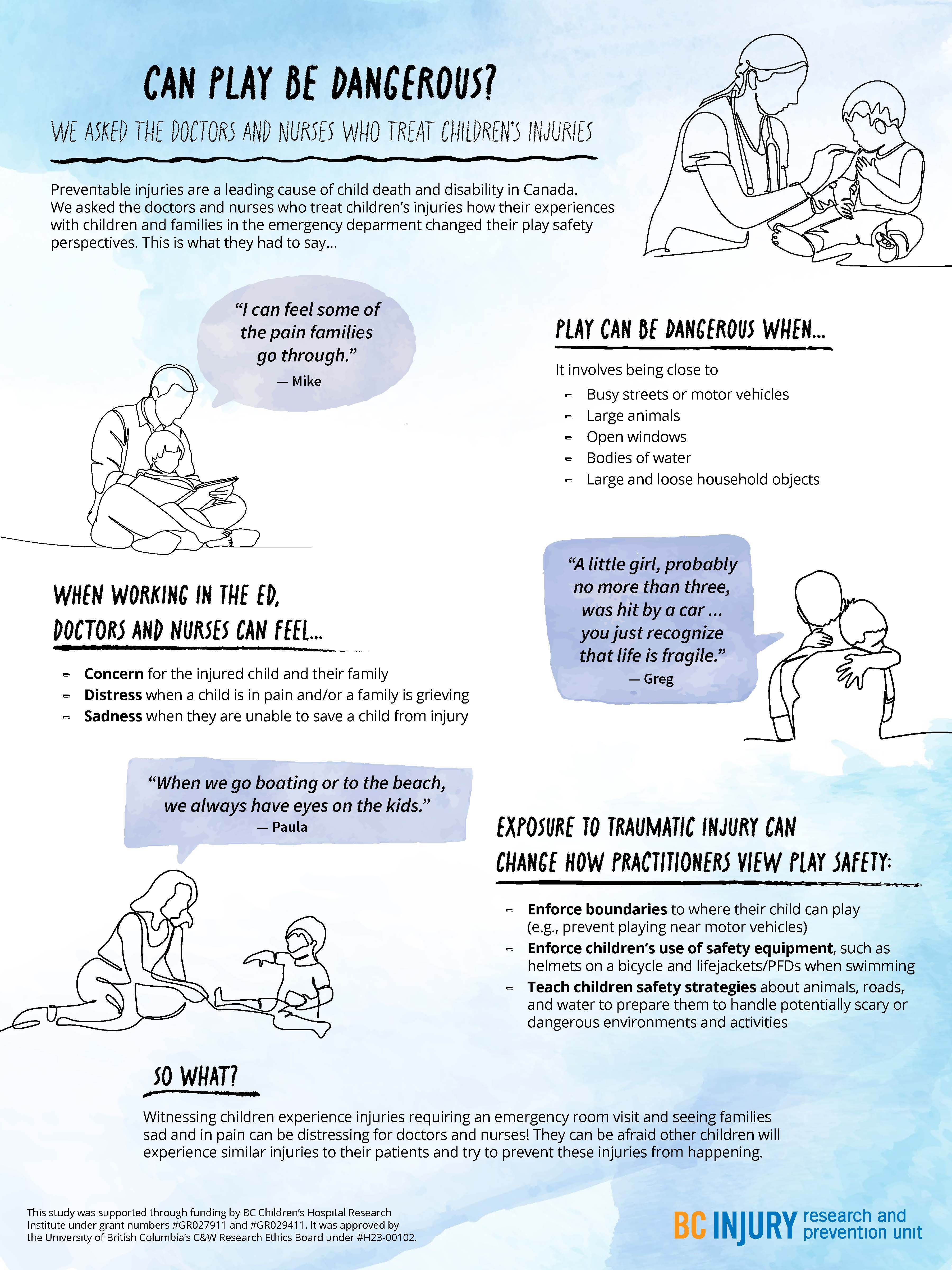
- distress when a child was in pain and when a family was grieving; and
- sadness in the event they were not able to save a child in their care.
- concern for the injured child and the child’s family;
Particularly traumatic events, such as those involving vivid sights and sounds (e.g., families holding each other and having extreme reactions), stuck with the practitioners, having long-lasting impressions on them and causing them to re-live these events in the years following their exposure.
Even after their shift was over, practitioners said that they changed how they approached parenting and how they perceived safety during play as a result of witnessing these traumatic events. They reported having more knowledge of the causes and consequences of severe injuries, such as those that require hospitalization or emergency care. For example, practitioners were more likely to enforce boundaries around where their children could play, such as by forbidding their child to play near busy streets. They also were more likely to tell their child about safe play environments and equipment, and put this equipment on their child before play, such as explaining the benefits of using helmets while riding bikes.
Practitioners were more likely to enforce boundaries around where their children could play, and use safety equipment, such as bike helmets.
Practitioners also described being concerned about their children’s play near open windows, around large bodies of water unsupervised, and in environments where firearms were present. They also expressed worry about their children’s play on trampolines and on motorized vehicles, such as ATVs. Findings related to trampoline play safety concerns were published in the journal Injury Prevention.
Observing family grief due to child injury or death affected the mental well-being of health care practitioners, drawing attention to the need for mental health supports for those involved in caring for severely injured and dying patients.

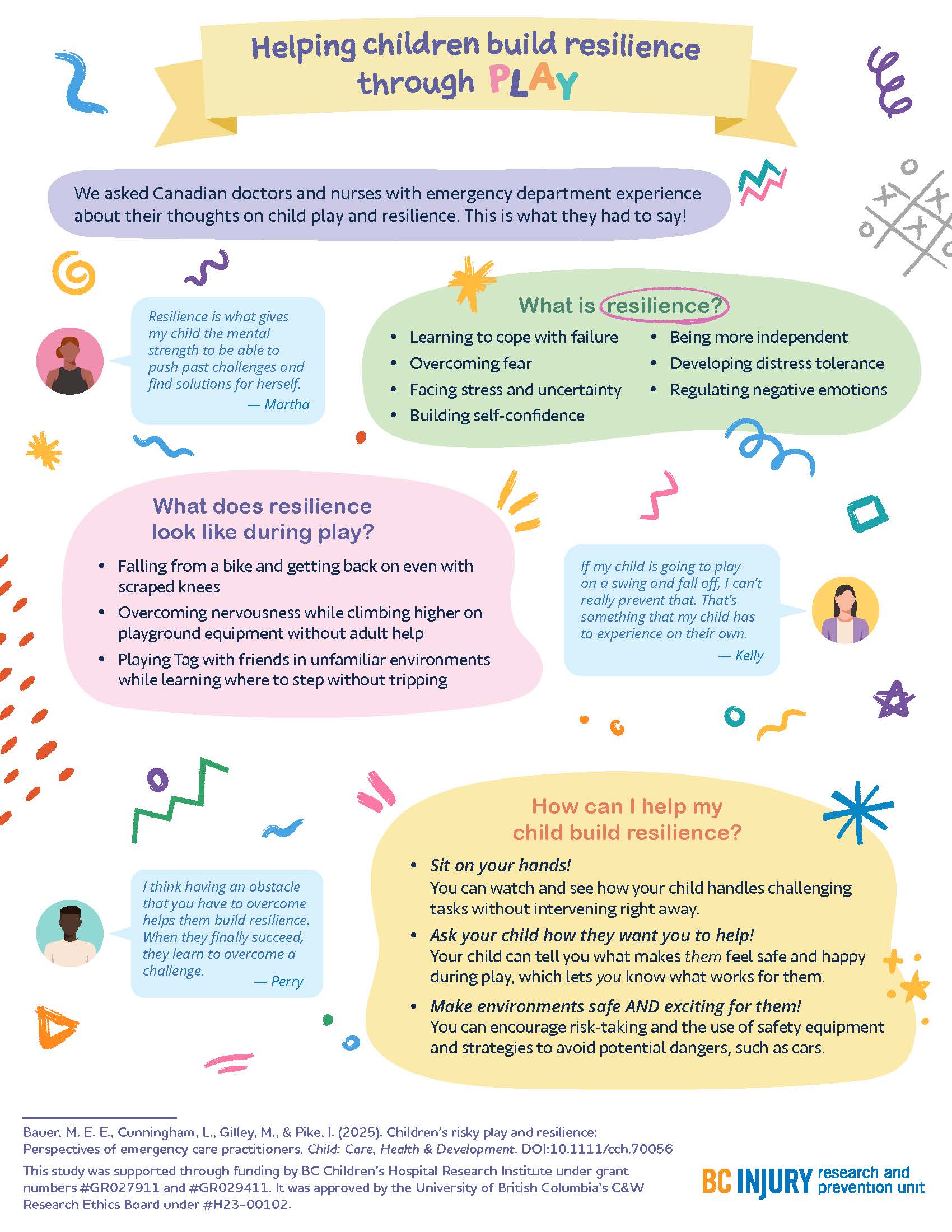
"Raise more resilient children through play...watch and see how your child handles challenging tasks without intervening right away." —Dr. Michelle Bauer
Building resilience through play
How can parents help their children build resilience? By letting them play!
The experiences that practitioners witnessed encouraged them to support their children in building resilience through play; specifically, by supporting children in learning to cope with failure, overcome fear, build self-confidence, develop distress tolerance, and regulate negative emotions. Findings related to building resilience through play were published in the journal Child: Care, Health, and Development.

Parents fostered resilience in their kids by:
- helping their kids get back on bikes after they fell off and wanted to try again;
- sitting on their hands so they did not instinctively reach for their children when their children fell down; and
- encouraging participation in challenging and thrilling activities in forests and water while safety equipment was used.
"There are a few ways that parents can raise more resilient children through play that are supported by literature and our study findings," said Dr. Bauer. "One: watch and see how your child handles challenging tasks without intervening right away."
"Two: Ask your child how they want you to help—let them tell you what makes them feel safe and happy during play. Let them lead. And three: make play both safe and exciting by encouraging risk-taking, teaching them how to avoid hazards, and using safety equipment.”
This research was supported through Drs. Bauer’s and Gilley’s receipt of a clinical and translational research seed grant from the BC Children’s Hospital Research Institute (BCCHR), Dr. Bauer’s BCCHR postdoctoral fellowship award, and additional training provided to Dr. Bauer through her participation in the Programs and Institutions Looking to Launch Academic Researchers (PILLAR) program through ENRICH, a national organization training perinatal and child health researchers.
Learn more about the study through two infographic posters:
Graphics and posters by Milica Radosavljevic