New BC clinical practice guideline for concussion and mild traumatic brain injury

A new resource is available to aid primary care physicians, nurse practitioners, and medical students in the assessment, diagnosis, and management of concussion/mild traumatic brain injury (mTBI).
The new clinical practice guideline is a practical tool to provide high-quality, timely, and appropriate care for people of all ages who may have sustained a concussion/mTBI. It contains key recommendations for assessment and diagnosis, management, follow-up, and special considerations. The Concussion Awareness Training Tool (CATT) e-learning courses and resources are recommended for use throughout the guideline, including the CATT for Medical Professionals course, which is an Accredited Self-Assessment Program (Section 3) as defined by the Maintenance of Certification Program of the Royal College of Physicians and Surgeons of Canada, and approved by UBC CPD.
The guideline was developed by the Guidelines and Protocol Advisory Committee (GPAC), an advisory to the BC Medical Services Commission, and in collaboration with key brain injury experts, including Drs. Shelina Babul, Paul Korn (Pediatric Medicine), Bryan Melnyk (Injury Prevention), Garth Meckler (Emergency Medicine), Noah Silverberg (Neuropsychology), and David Wilson (Family Medicine).
“This new clinical guideline is a much-needed resource to help primary care providers have an accessible reference to assess, diagnose, and manage concussion,” said Dr. Babul. “This guideline will allow patients to receive more timely and accurate care via their family doctor or emergency department.”
View the new guideline at BCGuidelines.ca.
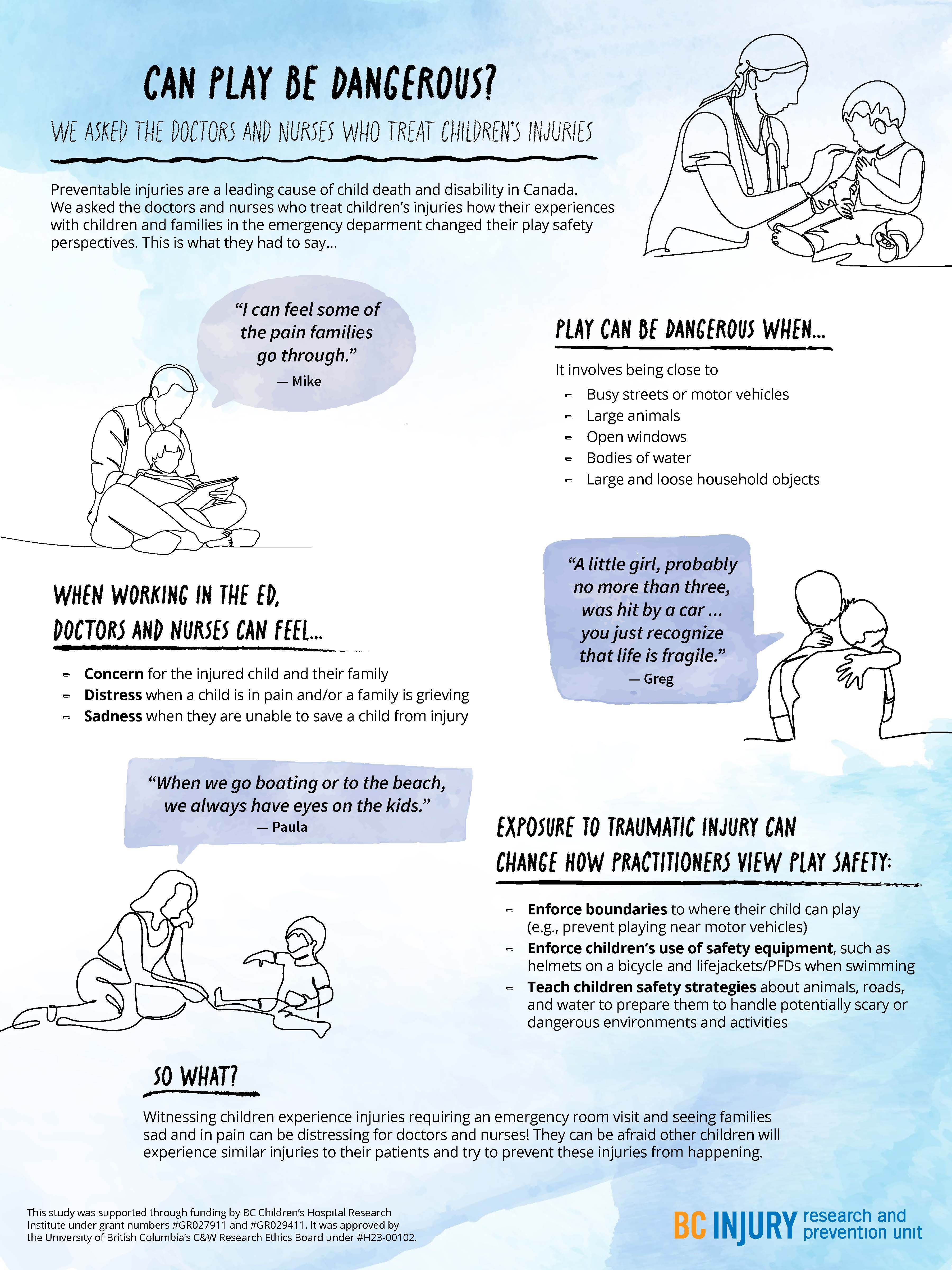
- distress when a child was in pain and when a family was grieving; and
- sadness in the event they were not able to save a child in their care.
- concern for the injured child and the child’s family;
Particularly traumatic events, such as those involving vivid sights and sounds (e.g., families holding each other and having extreme reactions), stuck with the practitioners, having long-lasting impressions on them and causing them to re-live these events in the years following their exposure.
Even after their shift was over, practitioners said that they changed how they approached parenting and how they perceived safety during play as a result of witnessing these traumatic events. They reported having more knowledge of the causes and consequences of severe injuries, such as those that require hospitalization or emergency care. For example, practitioners were more likely to enforce boundaries around where their children could play, such as by forbidding their child to play near busy streets. They also were more likely to tell their child about safe play environments and equipment, and put this equipment on their child before play, such as explaining the benefits of using helmets while riding bikes.
Practitioners were more likely to enforce boundaries around where their children could play, and use safety equipment, such as bike helmets.
Practitioners also described being concerned about their children’s play near open windows, around large bodies of water unsupervised, and in environments where firearms were present. They also expressed worry about their children’s play on trampolines and on motorized vehicles, such as ATVs. Findings related to trampoline play safety concerns were published in the journal Injury Prevention.
Observing family grief due to child injury or death affected the mental well-being of health care practitioners, drawing attention to the need for mental health supports for those involved in caring for severely injured and dying patients.

"Raise more resilient children through play...watch and see how your child handles challenging tasks without intervening right away." —Dr. Michelle Bauer
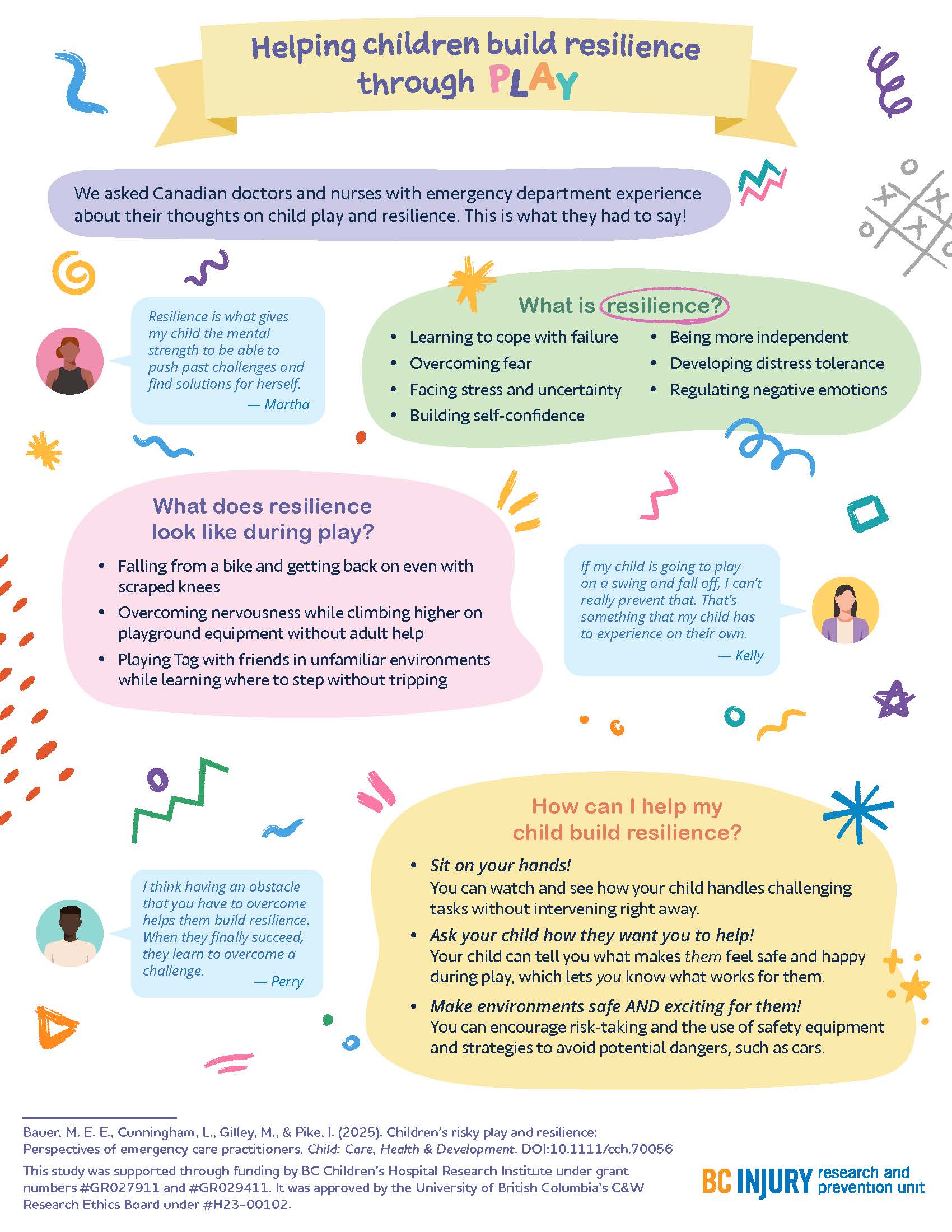
Building resilience through play
How can parents help their children build resilience? By letting them play!
The experiences that practitioners witnessed encouraged them to support their children in building resilience through play; specifically, by supporting children in learning to cope with failure, overcome fear, build self-confidence, develop distress tolerance, and regulate negative emotions. Findings related to building resilience through play were published in the journal Child: Care, Health, and Development.

Parents fostered resilience in their kids by:
- helping their kids get back on bikes after they fell off and wanted to try again;
- sitting on their hands so they did not instinctively reach for their children when their children fell down; and
- encouraging participation in challenging and thrilling activities in forests and water while safety equipment was used.
"There are a few ways that parents can raise more resilient children through play that are supported by literature and our study findings," said Dr. Bauer. "One: watch and see how your child handles challenging tasks without intervening right away."
"Two: Ask your child how they want you to help—let them tell you what makes them feel safe and happy during play. Let them lead. And three: make play both safe and exciting by encouraging risk-taking, teaching them how to avoid hazards, and using safety equipment.”
This research was supported through Drs. Bauer’s and Gilley’s receipt of a clinical and translational research seed grant from the BC Children’s Hospital Research Institute (BCCHR), Dr. Bauer’s BCCHR postdoctoral fellowship award, and additional training provided to Dr. Bauer through her participation in the Programs and Institutions Looking to Launch Academic Researchers (PILLAR) program through ENRICH, a national organization training perinatal and child health researchers.
Learn more about the study through two infographic posters:
Graphics and posters by Milica Radosavljevic